

All patients underwent multiple sleep latency test (MSLT) following nocturnal polysomnography (PSG). To ensure accurate diagnoses, cataplexy symptoms were confirmed through detailed clinical interviews by 2 or more board-certified physicians who are specialized in sleep medicine. NA/CA and NA w/o CA were diagnosed according to the criteria outlined in the ICSD-2. Twelve Japanese drug-naive patients having narcolepsy with cataplexy (NA/CA), 12 drug-naive patients having narcolepsy without cataplexy (NA w/o CA) and 12 non-obese healthy controls without EDS (NC) matched for age and sex were enrolled from April 2008 to December 2009 ( Table 1). All participant provided written informed consent before entering this study. This study was approved by the ethics committees of the Neuropsychiatric Research Institute. In the current study, we applied a voxel-based statistical approach to FA and ADC maps of patients having narcolepsy with and without cataplexy to evaluate brain microstructural differences. ADC values reflect microscopic water molecule diffusivity, and a high ADC value is thought to represent an increase in extracellular space and indicates microstructural changes in neurons. FA values represent tract directionality and integrity of neuronal fibers, being sensitive to the number, coherence, and degree of myelination of neural fibers. To the best of our knowledge, brain morphological and microstructural differences have never been studied in patients having narcolepsy with and without cataplexy.ĭiffusion tensor imaging (DTI) can identify the microstructural changes in neurons, as indicated by the values obtained for fractional anisotropy (FA) and apparent diffusion coefficient (ADC). However, all previous neuroimaging narcolepsy studies were conducted exclusively in patients with narcolepsy with cataplexy. This finding may suggest that the differences in clinical characteristics between narcolepsy with and without cataplexy are related to the difference in hypocretin fiber density in the anterior hypothalamus. A histopathological study indicated that hypocretin fiber density in the anterior hypothalamus was decreased in narcolepsy with cataplexy, but it was normal in narcolepsy without cataplexy. Narcolepsy without cataplexy differs from the former condition not only in terms of the absence of cataplexy but also in clinical (less severe EDS), biological (low CSF-hypocretin-1 levels in 10–20% of cases) and neurophysiological (lesser increase of REM sleep propensity) characteristics, –. In the second edition of the International Classification of Sleep Disorders (ICSD-2), narcolepsy was divided into 2 separate entities: i.e., narcolepsy with and without cataplexy.

Thus, brain morphometric changes in narcolepsy are still under debate. reported no differences in hypothalamic volume between patients with hypocretin-deficient narcolepsy and controls. reported volumetric changes mainly in hypothalamic gray matter and/or the frontal cortex. With regard to brain morphological studies on narcolepsy-cataplexy, Desseilles et al.
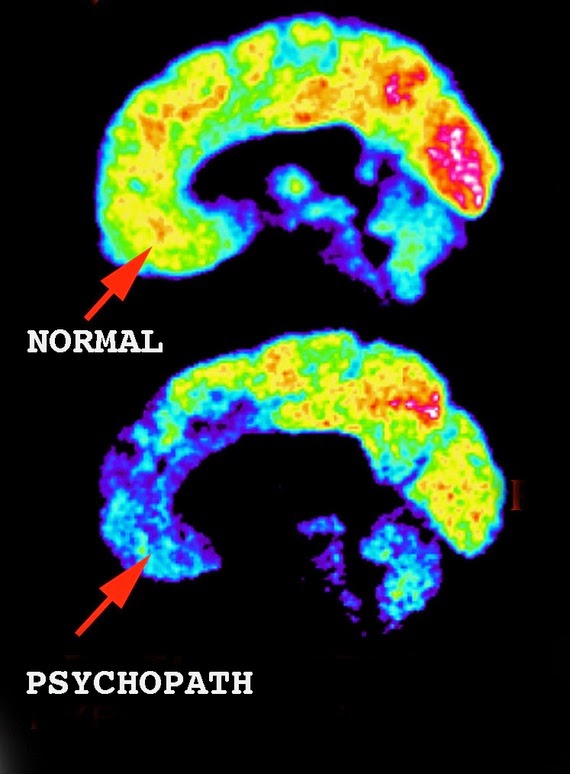
These studies have indicated that dysfunction of the midbrain and prefrontal cortices might be associated with narcolepsy pathology, however, the results were still conflicting. Furthermore, cerebral glucose Hypometabolism in the hypothalamic-thalamic-orbitofrontal pathways in narcolepsy was reported by Joo et al. In another study that used positron emission tomography (PET), cerebral perfusion was found to be reduced in the bilateral anterior hypothalami, prefrontal cortices, cingulated gyri, and many other midbrain structures. For example, in a study by Asenbaum et al., single photon emission computed tomography (SPECT) showed increased blood flow in the right hemisphere and decreased blood flow in the thalamus during REM sleep in patients with narcolepsy. Some Previous neuroimaging studies have attempted to clarify the mechanisms of the brain dysfunction in narcolepsy. Dysregulation of the hypocretinergic system plays an important role in the pathogenesis of human narcolepsy-cataplexy. Narcolepsy is a disabling sleep disorder characterized by excessive daytime sleepiness (EDS) and abnormal rapid eye movement(REM) sleep manifestations.


 0 kommentar(er)
0 kommentar(er)
